Silent strokes, often unnoticed and symptomless, pose a serious hidden threat to brain health. Unlike major strokes that show immediate signs, silent strokes quietly damage small areas of the brain, leading to long-term cognitive decline, memory loss, and increased risk of dementia. These “quiet attacks” often go undetected until significant neurological issues arise.
Understanding the causes, risk factors, and early detection methods is crucial to protecting your brain. Regular health checkups, managing blood pressure, and maintaining a healthy lifestyle can help prevent silent strokes and preserve cognitive function. Awareness is the first step toward safeguarding your brain’s future.
Table of Contents
- Introduction
- What Are Silent Strokes?
- How Silent Strokes Affect the Brain
- Causes and Risk Factors
- Symptoms: Subtle Signs You Shouldn’t Ignore
- Diagnosis and Detection Methods
- Prevention and Early Intervention
- Treatment and Recovery Options
- Silent Strokes and Dementia
- Conclusion
1. Introduction
In the realm of brain health, few conditions are as deceptive and underrecognized as silent strokes. While the term “stroke” typically conjures images of sudden paralysis, slurred speech, or dramatic collapse, a silent stroke operates very differently. It strikes quietly, without the telltale warning signs of a traditional stroke, yet it leaves behind lasting damage to the brain. Over time, these unnoticed attacks can contribute to cognitive decline, dementia, and physical impairment, often discovered only during a brain scan for unrelated issues.
In recent years, medical research has begun to unravel the true scope of silent strokes. Epidemiological studies suggest that one in four adults over the age of 65 has experienced at least one silent stroke, often without ever realizing it. This hidden prevalence makes silent strokes a global public health concern, especially as populations age and risk factors such as hypertension, diabetes, and cardiovascular disease become more common.
The real danger lies in their invisibility. Because silent strokes lack obvious symptoms, they often go untreated. The damaged brain tissue quietly accumulates over time, eroding memory, judgment, balance, and emotional control. For many, the first outward sign of a problem may be the onset of mild cognitive impairment or dementia, long after the initial damage occurred.
2. What Are Silent Strokes?
A silent stroke, also known as a silent cerebral infarct, occurs when the blood supply to a small part of the brain is interrupted, leading to cell death, but without causing any immediate, recognizable symptoms. Unlike major strokes, which affect large brain areas and manifest with clear signs like weakness or speech difficulties, silent strokes typically involve smaller blood vessels deep within the brain.
The result is localized damage that does not produce outward effects severe enough to alert the individual or observers. However, the brain tissue affected by a silent stroke still dies, leaving small scars or lesions visible on MRI or CT scans. Over time, these lesions can accumulate, interfering with neural pathways responsible for memory, coordination, and cognitive processing.
Silent strokes are most commonly categorized as ischemic, meaning they result from a blockage in a blood vessel, preventing oxygen and nutrients from reaching brain tissue. Hemorrhagic silent strokes, caused by small bleeds within the brain, are less common but can also occur, especially in individuals with uncontrolled hypertension or blood vessel abnormalities.
Despite their subtlety, silent strokes are anything but benign. Each incident represents irreversible damage to brain cells, and repeated events can lead to significant brain volume loss and impaired function.
3. How Silent Strokes Affect the Brain
The brain is an intricate network of billions of neurons communicating through complex electrical and chemical signals. Even minor disruptions in this network can have profound consequences. When a silent stroke cuts off the blood flow to a specific area, neurons in that region die within minutes due to lack of oxygen and glucose.
The location of the stroke determines the nature of its impact. For example:
- A silent stroke in the frontal lobe may subtly impair decision-making, concentration, or mood regulation.
- Damage to the basal ganglia can affect motor control and coordination.
- Lesions in the hippocampus or white matter tracts can compromise memory and cognitive speed.
Over time, multiple silent strokes contribute to what’s known as small vessel disease. A condition in which the brain’s tiny blood vessels become damaged, reducing overall blood flow and increasing vulnerability to further strokes. This cumulative effect can lead to vascular cognitive impairment, often mistaken for early Alzheimer’s disease.
Neuroimaging studies have shown that silent strokes can alter white matter integrity, disrupting the communication between different brain regions. These microstructural changes can translate into slowed thinking, difficulty multitasking, and emotional instability. Essentially, the brain becomes less efficient, forcing it to work harder to perform everyday functions.
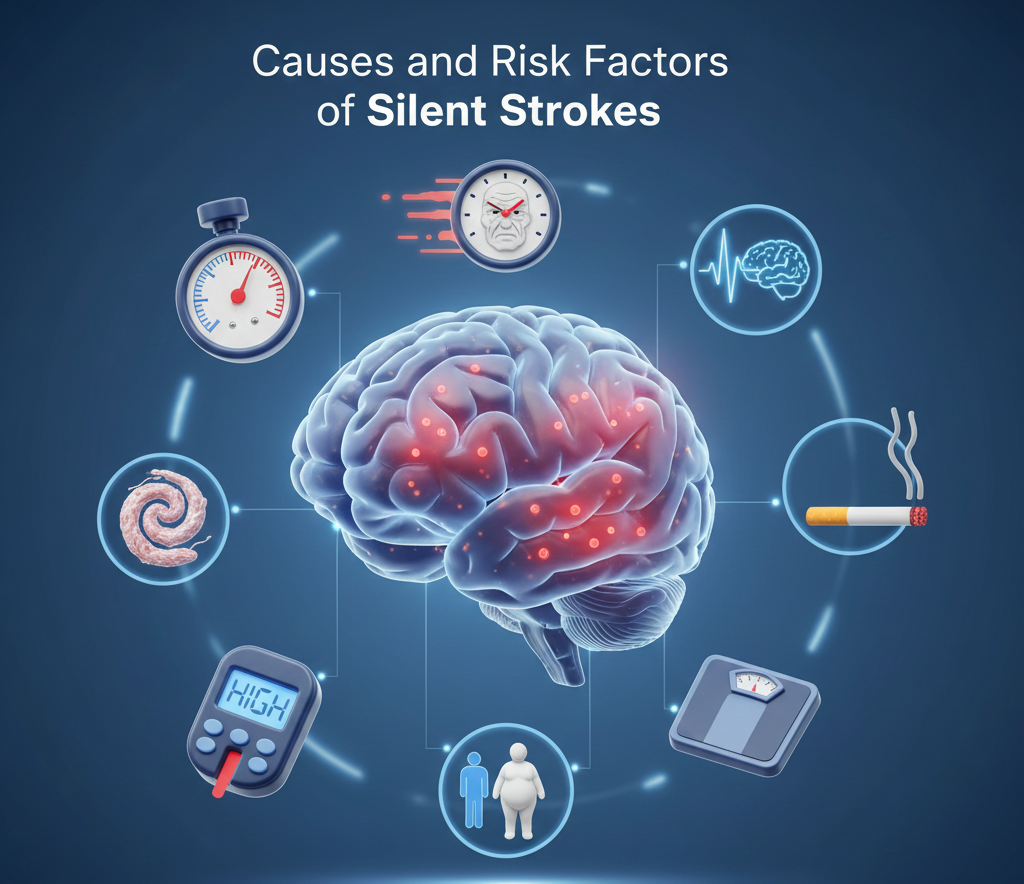
4. Causes and Risk Factors
Silent strokes share many of the same causes and risk factors as other types of strokes, particularly those linked to cardiovascular health. The underlying issue is typically reduced or interrupted blood flow to brain tissue due to vessel damage or blockage.
1) Hypertension (High Blood Pressure)
This is the leading risk factor for silent strokes. Chronic high blood pressure damages the walls of small arteries in the brain, making them prone to rupture or blockage.
2) Diabetes Mellitus
Diabetes contributes to vascular damage by promoting inflammation, thickening of vessel walls, and impaired circulation. It also increases the risk of clot formation.
3) Atherosclerosis
The buildup of plaque in arteries can restrict blood flow or cause emboli (blood clots) to travel to the brain, blocking smaller vessels.
4) Atrial Fibrillation (AFib)
An irregular heartbeat can lead to the formation of clots in the heart, which may dislodge and travel to the brain, causing silent infarcts.
5) Smoking and Excessive Alcohol Consumption
Both habits contribute to oxidative stress and vascular injury, increasing the likelihood of microvascular blockages.
6) Age and Genetic Predisposition
The risk of silent strokes rises sharply with age. Certain genetic factors affecting blood vessel health may also elevate risk.
7) High Cholesterol and Obesity
Excess cholesterol contributes to arterial plaque formation, while obesity increases the burden on the cardiovascular system.
8) Sleep Apnea and Sedentary Lifestyle
Interrupted breathing during sleep can cause blood pressure spikes, while lack of physical activity contributes to poor circulation and metabolic issues.
Collectively, these risk factors underscore the close relationship between heart health and brain health. What affects the cardiovascular system inevitably impacts the brain’s vascular network.
5. Symptoms: Subtle Signs You Shouldn’t Ignore
Silent strokes occur without noticeable symptoms, but that doesn’t mean they leave no trace at all. In some cases, subtle cognitive or physical changes may appear gradually, often dismissed as normal aging.
Some potential indicators include:
- Mild memory lapses or increased forgetfulness.
- Slight changes in mood or personality.
- Unexplained balance issues or unsteady walking.
- Decreased concentration or decision-making ability.
- Numbness or weakness in one part of the body that resolves quickly.
- A gradual decline in coordination or fine motor control.
Because these symptoms are often subtle and temporary, they rarely prompt immediate medical attention. However, they may signal that brain damage has occurred or is ongoing.
Importantly, individuals who experience Transient Ischemic Attacks (TIAs), sometimes called “mini strokes,” are at a particularly high risk. Although TIAs resolve quickly, they often precede silent or full-blown strokes.
6. Diagnosis and Detection Methods
Silent strokes are most often detected incidentally during imaging tests such as MRI or CT scans conducted for other reasons, like headaches or memory assessment. The lesions they leave behind are referred to as white matter hyperintensities (WMHs) or lacunar infarcts.
1) Magnetic Resonance Imaging (MRI)
MRI is the most sensitive tool for detecting silent strokes. It can reveal small areas of dead tissue or changes in white matter that indicate past vascular injury.
2) Computed Tomography (CT) Scan
CT scans are faster and more widely available but less sensitive than MRI for small infarcts. They can still reveal areas of brain tissue loss from prior strokes.
3) Cognitive and Neurological Assessments
Neurologists may perform memory, coordination, and reflex tests to evaluate subtle deficits related to silent strokes.
4) Blood and Cardiovascular Tests
Since silent strokes are closely tied to vascular health, doctors may check blood pressure, cholesterol levels, blood sugar, and heart rhythm to identify underlying risk factors.
Regular screening for individuals with high blood pressure, diabetes, or a history of cardiovascular disease can help detect silent strokes early before they lead to more serious consequences.
7. Prevention and Early Intervention
The good news is that silent strokes are largely preventable. Maintaining good vascular health through lifestyle and medical management can dramatically reduce risk. Prevention focuses on controlling modifiable risk factors.
1) Manage Blood Pressure
Keeping blood pressure within the normal range (<120/80 mmHg) is crucial. Regular monitoring, medication adherence, and dietary changes such as reducing salt intake are vital.
2) Control Blood Sugar Levels
For individuals with diabetes or prediabetes, maintaining healthy glucose levels through diet, exercise, and medication helps prevent vessel damage.
3) Quit Smoking and Limit Alcohol
Avoiding tobacco and keeping alcohol consumption moderate (or abstaining entirely) improves overall vascular function.
4) Eat a Brain-Healthy Diet
Diets rich in fruits, vegetables, whole grains, omega-3 fatty acids, and low-fat proteins (like the Mediterranean diet) protect blood vessels and reduce inflammation.
5) Exercise Regularly
At least 150 minutes of moderate exercise per week improves circulation, strengthens the heart, and enhances brain oxygenation.
6) Manage Weight and Cholesterol
Maintaining a healthy BMI and keeping LDL (“bad”) cholesterol low reduces arterial blockage risks.
7) Get Quality Sleep
Addressing sleep apnea and ensuring 7–8 hours of restful sleep per night supports vascular repair and reduces blood pressure fluctuations.
Early intervention also involves regular health checkups and discussions with healthcare providers about personalized risk management.
8. Treatment and Recovery Options
Once a silent stroke has occurred, the focus shifts to prevent future strokes and manage cognitive or neurological effects. While brain damage from a stroke is irreversible, rehabilitation and treatment can help preserve remaining brain function.
1) Medical Management
- Antiplatelet medications (e.g., aspirin) help prevent new clots.
- Antihypertensive drugs control blood pressure.
- Statins manage cholesterol levels.
- Anticoagulants may be used for those with atrial fibrillation.
2) Cognitive Rehabilitation
Therapists use exercises to improve memory, reasoning, and attention, helping the brain form new neural connections.
3) Physical Therapy
If balance or coordination is affected, physical therapy can restore mobility and reduce fall risk.
4) Lifestyle Modifications
Adopting sustainable habits for healthy eating, stress reduction, and consistent activity supports recovery and prevents progression.
9. Silent Strokes and Dementia
- One of the most concerning long-term consequences of silent strokes is their strong association with dementia. Research shows that individuals with silent cerebral infarcts are two to three times more likely to develop cognitive decline and dementia, particularly vascular dementia.
- Silent strokes damage white matter pathways essential for memory and communication between brain regions. As these networks deteriorate, cognitive processing slows, executive function declines, and memory lapses become frequent.
- Moreover, silent strokes can exacerbate the effects of Alzheimer’s disease, leading to a mixed form of dementia that progresses more rapidly. The dual impact of vascular and neurodegenerative damage makes prevention and early detection vital.
10. Conclusion
Silent strokes represent a hidden but pervasive threat to global brain health. Their lack of symptoms often means they go unnoticed until significant cognitive or neurological impairment appears. However, knowledge and awareness can transform outcomes.
By understanding the risk factors, recognizing subtle warning signs, and prioritizing cardiovascular and neurological health, individuals can take control of their long-term well-being. Regular medical checkups, imaging when indicated, and proactive lifestyle choices form the cornerstone of prevention.
The message is clear: what the brain suffers in silence can have loud consequences later in life. Early intervention, education, and awareness are our best defenses against this quiet epidemic. Protecting brain health isn’t just about avoiding catastrophic strokes. It’s about preventing silent ones that quietly steal our vitality, memory, and independence.